Let’s walk through a case from start to finish. I’ll put more emphasis on the surgical phase and just outline the restorative phase.
Tammy is like many of our patients. She is fearful of dentists and only visits when things are hurting. Tammy came to our office for limited exam (emergency visit) to evaluate her broken upper left first molar (#14). Our brief exam revealed a significant fracture of the mesiolingual cusp #14 and heavy calculus buildup.

Based on the clinical finding our treatment plan was for the removal of #14 to deal with her chief complaint. I also expressed concern regarding her overall gum health and recommended full mouth scaling and root planing.
Tammy’s first question was how long would she have to go without a tooth and how many visits this would take. My answers were that I could complete her care in two visits about 4 months apart and she would only be without a tooth for that time period.
Her next question was how do you do this and make me comfortable. To this I answered that we offer oral sedation.
Her final question was how much and how does she pay for it. To this, I invited our treatment coordinator into the room and went over the details of our visit and Melinda put together a written plan and written financial arrangements for Tammy.
Tammy agreed to treatment and selected our in office no interest 6 month payment plan. Her first visit would be full mouth scaling and root planing with our hygienist and then extraction/implant with myself in a single visit.
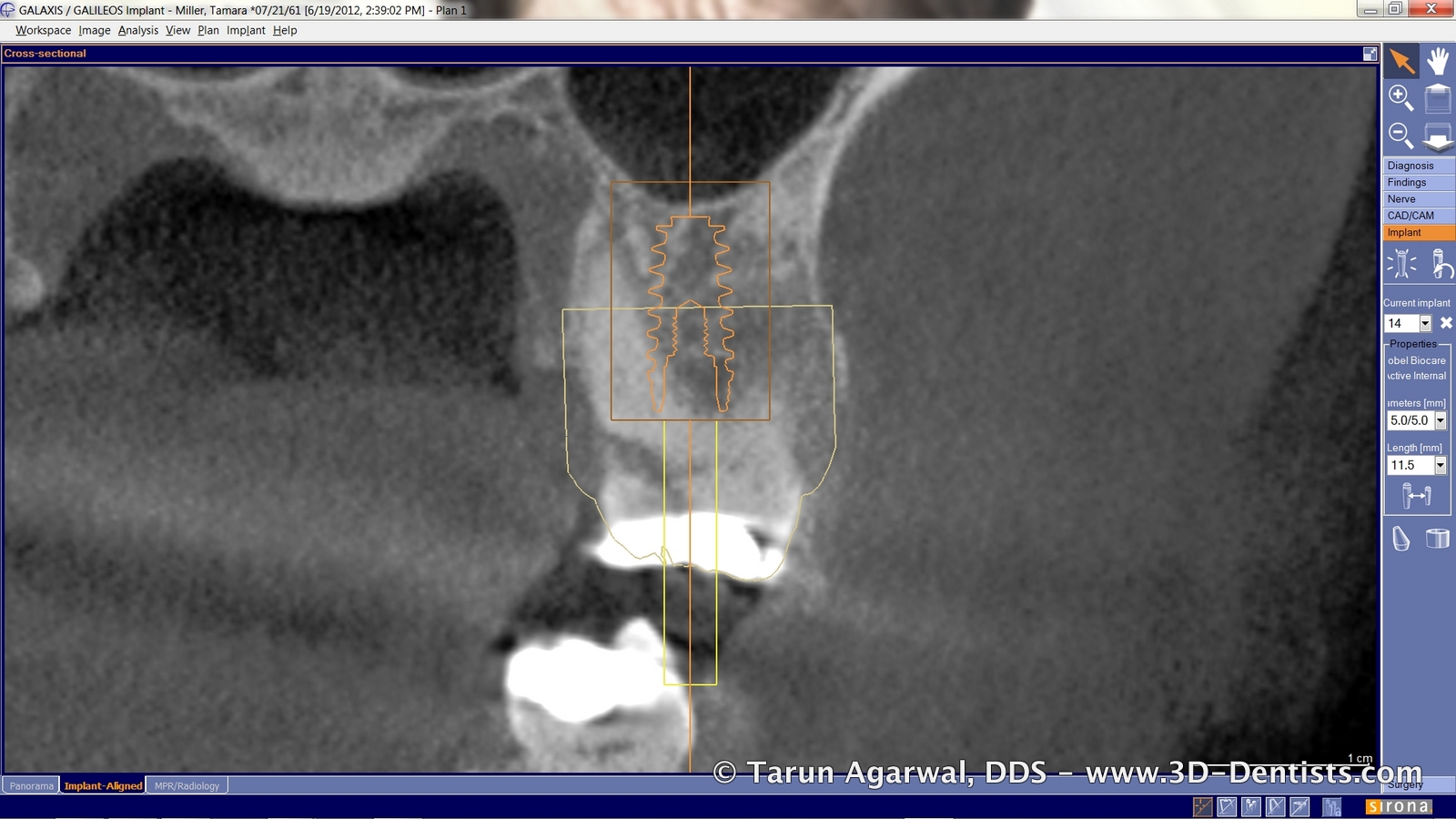
Between her emergency visit and her treatment visit, I finalized her implant plan and ordered a surgical guide for implant placement.



Her implant planning showed sufficient bone to allow for immediate placement. I recognized that we were going to be close, if not into, the sinus so we were prepared for a minor sinus bump.
Immediate placement is predicated upon removing the tooth ‘atraumatically’ and not damaging the bone. My preferred method of extraction for immediate placement is to section the tooth and remove each root individually.


Once the tooth is removed and the site debrided, the surgical guide is placed and the ostotomy completed. In the case of maxillary molars (softer bone), I will purposely undersize the osteotomy to preserve bone and gain stability. This concept is predicated on using an active implant that is self tapping and condensing.


Since we were quite close to the sinus, I removed the surgical guide, flushed the osteotomy to remove any debris. I gently ‘up fractured’ the floor of the sins with an osteotome. I then went ahead and placed particulate bone into the extraction sockets and into the osteotomy.

The surgical guide is then placed back into the mouth and the implant is driven into place.



My preferred implant is the NobelActive. I prefer this implant because it is end cutting and condenses the bone. I find that I can almost always attain primary stability with this implant. It will also divert the particulate bone into the nooks and crannies of the site. In this case it also drove the graft material slightly into the sinus for my internal sinus lift.

A collagen plug was used to cover the site and several sutures were placed to hold it all together.

Patient returned for a brief check at the 2 week mark. At this visit we also went ahead and scheduled Tammy for a single visit implant restoration visit at the 6 month mark. This would also coincide with one of her perio maintenance visits.

At her six month visit, prior to beginning restorative treatment the site is evaluated clinically and radiographically.


Since there is a large band of keratinized tissue – a benefit of immediate placement with ‘gap’ grafting is the preservation of the site dimensions. A punch was used to uncover the implant. A slight amount of lidocaine is given directly to the crystal tissue and the surgical guide is used to punch the tissue.


A digital impression post is placed onto the implant and scanned with CEREC to fabricate the idealized screw retained implant restoration.


After the restoration is milled and stain/glazed it is bonded to the TiBase and delivered to the patient.